SCIENCE
Abarceo Pharma is a spin-out of Lund University Diabetes Center founded in 2017 by Prof. Claes Wollheim, MD, and Associate Prof. Albert Salehi world-renowned scientists in diabetes research and beta-cell biology. Abarceo Pharma has identified a novel diabetes target VDAC1 located on beta cells and a novel mechanism of action enabling a therapeutic treatment to revert beta cells from dysfunctional to functional, preserving beta cell function and allowing patients to produce their insulin again, naturally. The company founders were the first to describe that voltage-dependent anion channel 1 (VDAC1) is dysfunctional and presents a novel target in Type 2 Diabetes (T2D). VDAC1 is a key mitochondrial protein regulating the energy production in cells and has been implicated in multiple diseases with underlying mitochondrial dysfunction including neurodegenerative and cardiovascular disease (CVD). These diseases are closely related to T2D and are often referred to as comorbidities.
Abarceo Pharma is developing a small molecule technology platform for the treatment of mitochondrial dysfunction, with an initial focus on T2D.
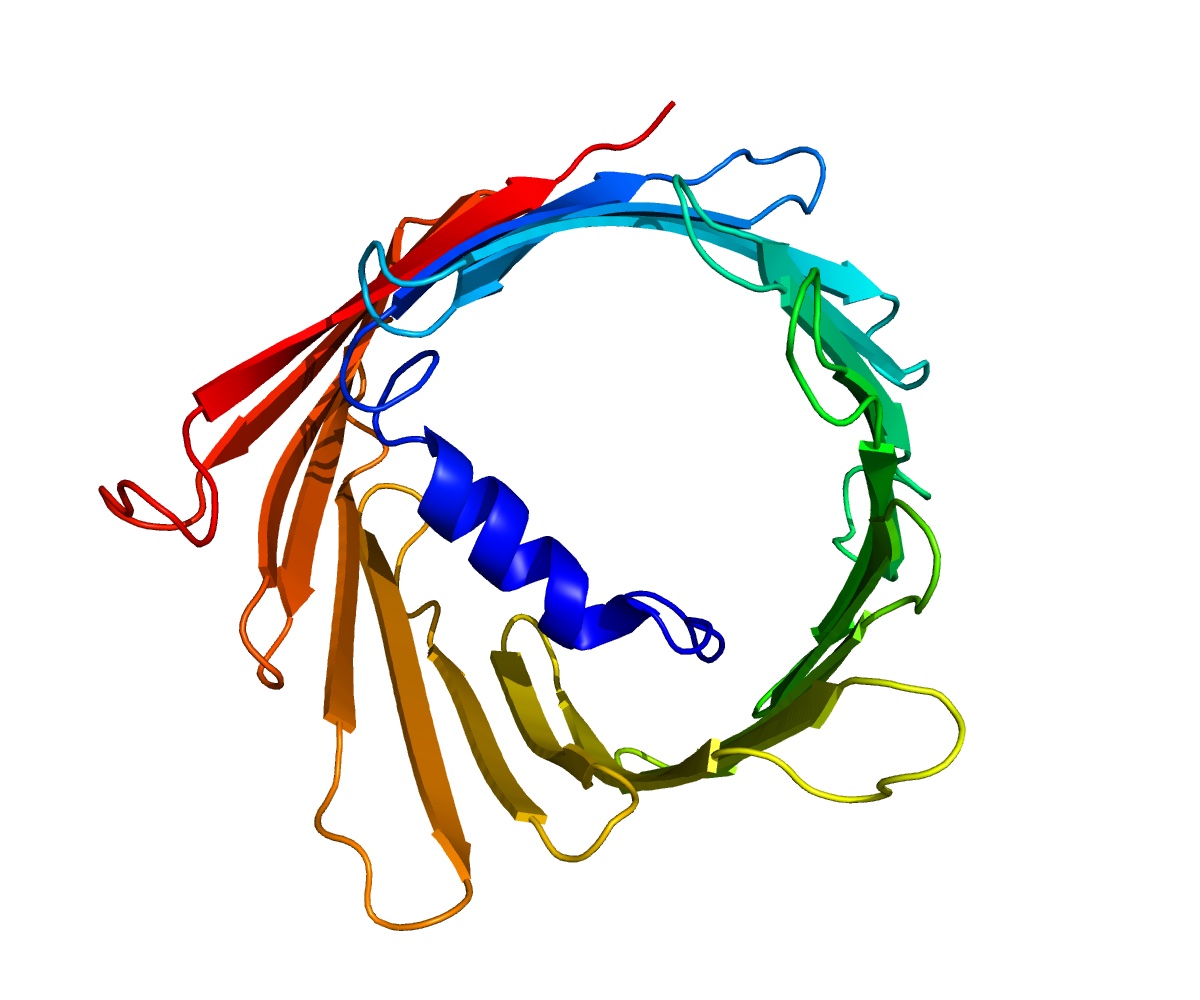
Voltage-dependent Anion Channel 1 (VDAC1)
VDAC1 is an ion channel located in the outer mitochondrial membrane where it allows the energy-carrying molecule ATP (adenosine triphosphate) to diffuse out of the mitochondria into the cytoplasm. In the healthy state, VDAC-1 allows for communication between the mitochondrion and the cell, controlling energy, but also mediating the balance between cell metabolism and cell death (apoptosis)4,5. VDAC1 regulates apoptosis by orchestrating the release of apoptotic proteins from the mitochondria. Under normal healthy conditions, VDAC1 exists as a highly-tuned single-molecule channel (monomer). But in many mitochondrial pathological conditions cell death occurs via VDAC1 overexpression and oligomerization (clustering of several VDAC1 molecules) resulting in the formation of a large channel leaking out ATP and cell death signaling molecules6. In T2D, VDAC1 is found to be overexpressed and abnormally localized to the outer membrane of the beta cell, causing ATP leakage and subsequent insulin secretion dysfunction. The ATP leakage is believed to be the underlying cause of the “sleeping” beta cells not having enough energy to secrete sufficient levels of insulin in T2D (see the middle section in Figure below). Abarceo researchers have described that insulin secretion in T2D can be restored by inhibiting VDAC1 overexpression and blocking VDAC1 at the beta-cell plasma membrane. The apoptosis and ATP loss, causing beta-cell dysfunction in T2D, was found to be blocked by VDAC1 modifiers. (Abarceo Lead, see Figure below). This discovery links to the underlying mitochondrial dysfunction and energy loss which has been implicated in a wide range of diseases in addition to diabetes including cardiovascular and neurodegenerative diseases such as Alzheimer’s
Type 2 Diabetes – a pandemic affecting 1 in 10 adults
T2D is a metabolic disorder which is characterized by hyperglycemia (unhealthy high levels of blood glucose). The cause for T2D is unclear but genetics, overweight and sedentary lifestyle are known contributing factors that lead to insufficient insulin secretion and deteriorating insulin sensitivity. Insulin is produced by the “beta cells” that are part of a cell cluster called the Islets of Langerhans. Abarceo scientists have delineated how, in T2D patients, the beta cells are dysfunctional and do not respond to high glucose as healthy cells would1
• The global prevalence of T2D is rising dramatically.
• The disease is currently affecting more than 500 million people and predictions are it will impact lives of nearly 800 million by 20452.
• This pandemic is driven by increased urbanization, lifestyle changes including increased consumption of sugar and sedentary lifestyles, population growth, and aging populations.
• Close to 7 million deaths in 2021 can be attributed to diabetes2
A staggering 12% of global health costs are spent on diabetes and its comorbidities
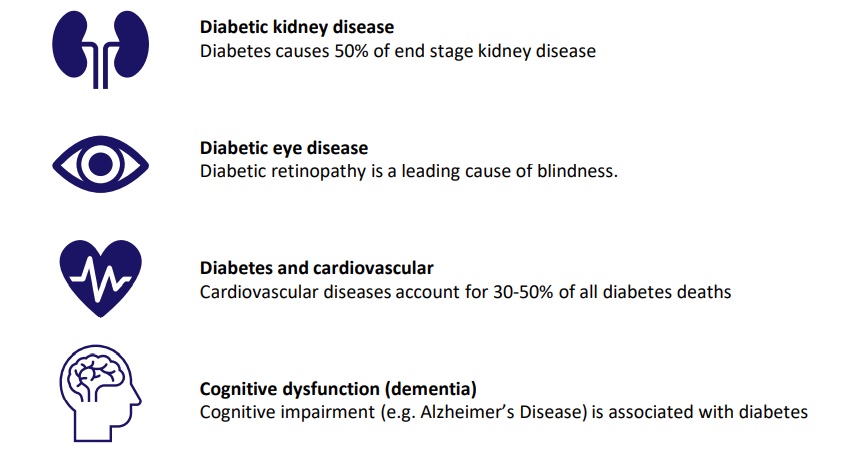
Abarceo’s treatment holds the promise of improved therapeutic sustainable blood glucose control in addition to its direct on-target effect on dysfunctional VDAC1 in tissues/organs involved in T2D complications, with the added benefit of no risk of hypoglycemia. Abarceo’s technology platform provides the first disease-modifying treatment option offering more quality years to patients, and significant less burden on the health care system as fewer patients will develop the dreaded late-stage complications (comorbidities), once the degeneration process has started.
Mitochondrial and VDAC1 dysfunction in chronic diseases beyond T2D
Emerging data show that blocking dysfunctional VDAC1 can have effect in diseases with underlying mitochondrial dysfunction7. Mitochondrial dysfunction is known to be associated with a wide range of human pathologies, such as neurodegenerative diseases, cardiovascular diseases, autoimmune diseases and cancer. Abarceo’s strategy is to continue to establish Preclinical Proof of Concept in models of Alzheimer’s Disease (AD) and Acute myocardial infarction (AMI), two indications with strong scientific evidence of VDAC1 overexpression and mitochondrial dysfunction. Exploring these two opportunities represents a potential and huge impact on the treatment of devastating diseases that burden the world’s economies and human health in addition to the personal impact on the patients and relatives’ lives. Alzheimer’s Disease Dementia (AD; the most common form) affects approximately 50 million people globally and is expected to triple by 2050. Market size is currently USD 6 billion and expected to pass USD 12 billion by 2028. Ageing and T2D are strong contributing factors to the increase in cases in all geographies14. There is no effective treatments on the market which can sustainably slow disease progression. Most AD strategies are addressing either tau or beta-amyloid plaques malignancies but have shown disappointing results in clinical testing. In this setting Abarceo’s platform technology represents a completely novel approach to treatment of AD by restoring healthy mitochondria in the brain. Acute myocardial infarction (AMI) Myocardial infarction (heart attack) is the irreversible death of heart muscle due to prolonged lack of oxygen supply. Acute myocardial infarction is one of the leading causes of death in the developed world and approximately 1.5 million cases of AMI occur annually in the United States15. At least 50% of T2D patients have cardiovascular complications and of these approximately 20% get AMI. The mortality from AMI was estimated to be 2.5 times higher in T2D than in non-diabetic subjects16.